Atrial fibrillation (AFib) is an irregular and often rapid heart rate that can increase your risk of stroke, heart failure and other heart-related complications. This irregular heart rhythm can lead to symptoms that negatively impact the quality of life in some people. Others experience no symptoms at all. During atrial fibrillation, the heart’s two upper chambers (the atria) beat chaotically, rapidly and irregularly out of coordination with the two lower chambers (the ventricles) of the heart. Atrial fibrillation symptoms often include heart palpitations, shortness of breath, dizziness, fatigue and weakness. When AFib occurs, the electrical impulse does not follow the normal order. Instead of one impulse moving through the heart, many impulses begin in the atria and fight to get through the AV node. This happens for two reasons: First, the structure of the heart and its electrical pathway may change over time; this happens more often as we get older. Second, as the electrical pathway changes, one or more “triggers” may develop. “Triggers” are electrical circuits that send extra impulses at a faster than usual rate.
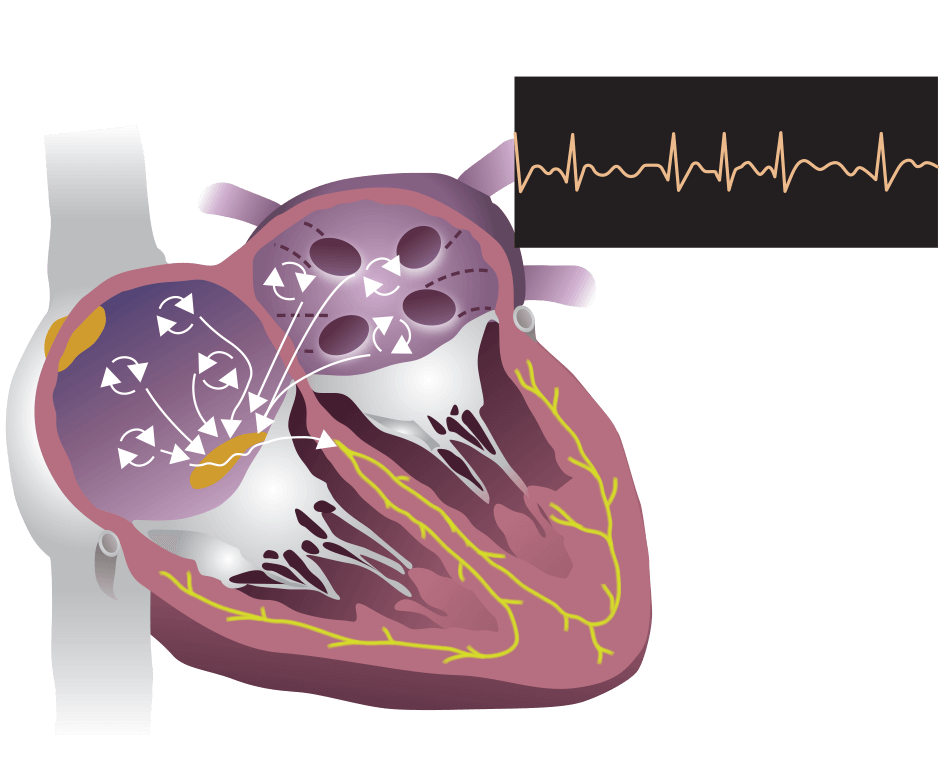
Atrial Fibrillation Heart Rhythm, Courtesy of Medtronic.
These extra impulses are all trying to get through the AV node and the atria begin to fibrillate, quiver or twitch, in a fast and disorganized way. Treatments for atrial fibrillation may include medications and other interventions to try to alter the heart’s electrical system. Since other heart disorders increase the risk of developing abnormal heart rhythms, lifestyle changes often are recommended. Living a “heart healthy” lifestyle can ease the symptoms experienced with heart rhythm disorders and other heart disorders, and can be beneficial to overall patient health. Devices that “pace” the heart rate when it is too slow (bradycardia) can take over for the heart’s natural pacemaker, the sinoatrial node, when it is not working properly. Pacemakers monitor and regulate the rhythm of the heart and send electrical signals to stimulate the heart if it is beating too slowly.
